It has been suggested that research studies informing third stage of labour practice guidelines and recommendations are questionable, particularly for women at low risk of postpartum haemorrhage who choose to birth in midwife-led units or home birth settings (Baker et al, 2021). This article discusses the findings from a literature review conducted in June 2021 and updated in August 2021, to answer the question of whether there are any published studies that have investigated active verse expectant management of the third stage of labour, and any related blood loss during this period or shortly after, in women who had a normal physiological birth and gave birth or intended to give birth in a midwife-led unit.
Active third stage of labour management approach in this study refers to acceleration of the delivery of the placenta to reduce blood loss using a prophylactic uterotonic drug (exogenous oxytocin) to accelerate the contractility of the uterus, causing the placenta to separate from the uterus wall more quickly. Other components of active management in this study may also include delayed or immediate cord clamping and controlled cord traction (National Institute for Health and Care Excellence (NICE), 2017; Royal College of Obstetricians and Gynaecologists (RCOG), 2016).
Expectant management is also known as physiological, passive, or conservative management. This approach consists of supporting a woman's body to physiologically birth her placenta. No routine use of uterotonic drug is involved. No clamping of the cord takes place until the cord has stopped pulsating and delivery of the placenta is by gravity or maternal effort.
A postpartum haemorrhage in this study is defined as bleeding from the genital tract of 500 mL or more after the birth of the baby or shortly afterwards. Severe postpartum haemorrhage was defined as blood loss of 1000 mL or more after the birth of the baby or shortly afterwards.
The midwife-led unit is where normal labour and birth are promoted, and women are cared for by midwives. These midwives are sometimes supported by maternity support staff. There is no routine input by obstetric staff, as women who birth in midwifeled units are ideally classified as at low risk of obstetric complications. If complications occur during childbirth or shortly afterwards, the woman will need to be transferred to an obstetric-led unit.
Concerns about how the physical environment of an obstetric-led unit can affect the development of complications during childbirth and influence women's satisfaction with care have been voiced (Hodnett et al, 2012). Research studies have reported many beneficial outcomes for healthy women at low risk of obstetric complications who plan to give birth away from hospital obstetric-led units, particularly for women who choose to birth in midwife-led units (Brocklehurst et al, 2011; Hollowell et al, 2011; Hodnett et al, 2012; Christensen and Overgaard, 2017). The beneficial outcomes of birthing away from a hospital obstetric-led unit may arise as a result of midwife-led units and home birth setting promoting active labour and birth. Additionally, women are cared for by midwives, as they are ideally classified as at low risk of obstetric complications and prefer little or no intervention in the birthing process.
Search strategy
The PICOS (Population, Intervention, Comparison and Outcomes, Study) tool was used as a structure to organise a list of terms, addressing the main issues in the research question (Table 1).
Table 1. PICOS tool to organise a list of terms
| Population | Women receiving midwifery-led care, women giving birth in alternative institutional settings, midwifery-led care, midwife-led care alternative birth setting, alternative institutional birth setting, birth centres, birth centre, midwifery-led unit, midwife-led unit, midwifery unit |
| Intervention | Third stage, active management, expectant management, physiological management |
| Comparison | None identified at this stage |
| Outcomes | Blood loss, postpartum haemorrhage, postpartum haemorrhage |
| Study | Primary study, quantitative study |
The PICOS tool and its terms were then used to search electronic databases. To ensure the most comprehensive and unbiased searches possible, advanced searches were conducted on the most relevant electronic databases used for medical and midwifery research:
- EMBASE (Excerpta Medica Database)
- Psych Info (Psychology and allied fields)
- AMED (Allied and Complementary Medicine)
- HBE (Health Business Elite)
- PubMed
- BNI (British Nursing Index)
- HMIC (Health Management Infor mation Consortium)
- CINAHL (Cumulative Index to Nursing and Allied Health Literature) and Medline).
No date was set when searching the electronic databases for studies, to avoid unnecessary contraints on the search. Reference lists from relevant studies were reviewed, hand searches were conducted on the last 2 years' editions of the most frequently cited journals and key midwifery and medical journals (British Journal of Midwifery; Midwifery; Journal of Advanced Nursing; Birth and Women and Birth). This time limit was set as although hand-searching may supplement structured documented searches because of, for example, incomplete indexing, it is a time-consuming process not practical to implement over an extended time range. Moreover, the extent of the systematic searching should limit the additional benefit of hand searching. Relevant internet resources were also searched (NICE; Cochrane Library; World Health Organization (WHO); RCOG) for possible studies for this literature review.
Study selection
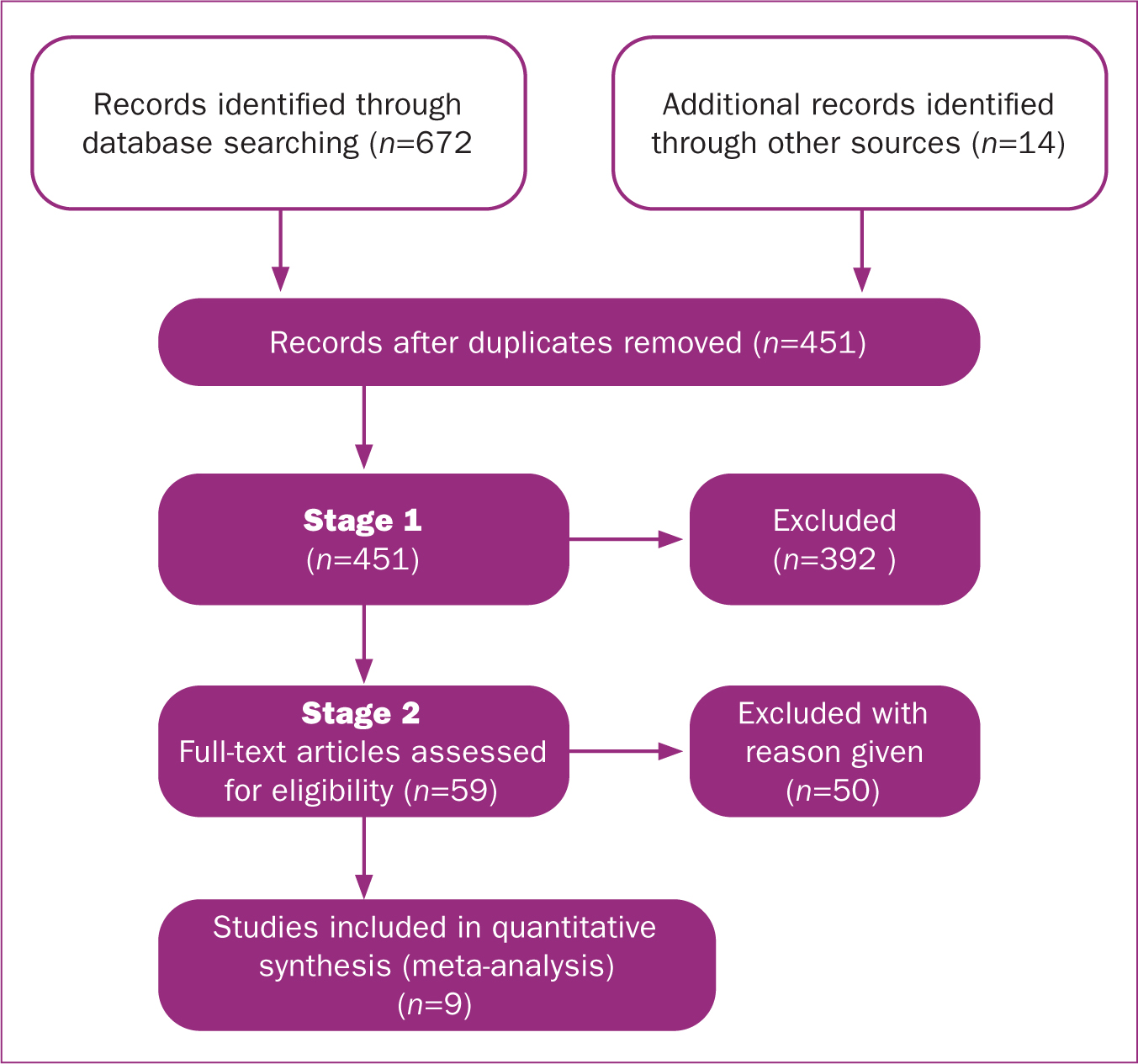
From the electronic database results, study selection was then conducted in two stages to increase the transparency of the study selection process (Centre for Reviews and Dissemination, 2009; University of York, 2021). An initial screening of titles and, where possible, abstracts, was conducted against pre-determined inclusion criteria. Then all the research study papers that appeared to meet the pre-determined inclusion criteria, or those that were ambiguous, were obtained in full and screened by the author against the pre-determined inclusion criteria (Table 2).
Table 2. Pre-determined inclusion and exclusion criteria
| PICOS element | Inclusion | Exclusion | Justification for exclusion |
|---|---|---|---|
| Population | Studies that define pregnant women as being at low risk of postpartum haemorrhage birthing in midwife-led units.Studies where data on outcomes was presented separately for different places of birth, so that outcome for midwife-led units compared to other settings was evident | Studies with pregnant women at high risk of postpartum haemorrhage.Women in low-income countries who did not give birth in midwife-led units.Women not birthing or planning to birth in midwife-led units | Including studies containing women at increased risk of postpartum haemorrhage would bias results and reduce generalisability of findings to low-risk women in high-income countries.Place of birth has been shown to influence birth outcomes |
| Intervention | Studies that define active management of third stage of labour as using a prophylactic uterotonic drug to accelerate contractility of the uterus. Other components may also have included delayed or immediate cord clamping and controlled cord traction.Studies that defined expectant management of third stage of labour as no routine use of uterotonic drug. No clamping of cord until cord has stopped pulsating and delivery of placenta by gravity or maternal effort. | Studies that do not use oxytocin or syntometrine as routine prophylactic uterotonic drugs | Oxytocin or syntometrine are the pharmacologic agents currently used in high-income countries for active management of third stage of labour |
| Comparison | Studies that compare active versus expectant management of third stage of labour | Any interaction that does not compare active versus expectant management of the third stage of labour | This systematic review aims to compare active versus expectant management and not any other management approaches |
| Outcome | Studies that report postpartum haemorrhage and blood loss after birth as estimated by practitioner by visual estimation or weighed.Studies that report treatment received for excessive blood loss. | Studies that do not measure blood loss | Postpartum haemorrhage or excessive bleeding at/after childbirth is potentially life-threatening and a major contributor to maternal mortality and morbidity |
| Study design | Primary published quantitative research studies-reviews, randomised controlled trials and observational studies (cohort and case control studies).No date restrictions.Research articles in English | Unpublished research studies.Qualitative studies | Obtaining unpublished research studies can be time-consuming and original data may no longer be available |
Research studies identified by looking at reference lists from relevant studies, hand-searching the most frequently cited journals and key midwifery and medical journals and searching relevant Internet resources were then assessed for inclusion in the review against the pre-determined inclusion criteria.
Results
A total of 686 research study papers were identified, with 451 remaining after removal of duplicates. After screening the titles and abstracts, 59 papers remained. After reading the full text, nine papers appeared to meet the inclusion criteria (Figure 1):
- Begley et al, 2011a
- Davis et al, 2012
- Dixon et al, 2009
- Dixon et al, 2014
- Fahy et al, 2010
- Grigg et al, 2017
- Kataoka et al, 2018
- Laws et al, 2014
- Monk et al, 2014.
These papers were critically reviewed using a Critical Appraisal Skills Programme (2018) tool and were judged to be of high enough quality to be included.
All included studies compared, directly or indirectly, active versus expectant third stage management approaches for women at low risk of postpartum haemorrhage giving birth in midwife-led units, in terms of blood loss during the third stage of labour and shortly thereafter. The studies included one randomised controlled trial (Begley et al, 2011a), with the remainder being prospective or retrospective cohort studies.
Outline and critique of identified papers
Davis et al (2012) investigated the effect of planned place of birth on the risk of severe postpartum haemorrhage (defined as blood loss of more than 1000 mL) and active compared with expectant management of the third stage of labour. The study analysed data collected from the New Zealand College of Midwives' research database for women giving birth in 2006 and 2007, who were classified as at low risk of postpartum haemorrhage when labour commenced. Data were obtained for 39 677 births, of which 16 453 (41.5%) met the study criteria. Outcomes were attributed to the planned place of birth at the onset of labour. The study found that the proportion of women who had a severe postpartum haemorrhage was higher in women who received active management compared to those who received expectant management in all birth settings, (relative risk: 2.14, 95% confidence interval: 1.42–3.22). Women who received active management in primary level units (midwife-led units) were more than twice as likely to have a severe postpartum haemorrhage as women who received expectant management (1.7% (23 women) versus 0.6% (9 women)). However, twice as many women in the expectant management group went on to have further (uterotonic) treatment for excessive blood loss compared with those in the active management group (14.0% vs 7.3%).
Dixon et al (2009) also analysed data collected from the New Zealand College of Midwives' research database, comparing active and expectant management of the third stage of labour for all normal physiological births from 2004 to 2008. A total of 33 752 women met the study inclusion criteria. The study found that primary level units experienced a reduction in the occurrence of postpartum haemorrhage, despite an increase in the use of expectant management (57.8%) compared to active management (42.2%). This was in comparison to the secondary and tertiary level units (obstetric-led units), which reported an increased proportion of active management (63.7% and 65.7% respectively) compared to expectant management (36.3% and 34.1 respectively). The proportion of blood loss of 501–1000 mL was 4.1% and 0.99% for a blood loss greater than 1000 mL at the primary level unit. At the secondary and tertiary level units (obstetric-led units), the proportions of blood loss of 501–1000 mL were 4.2% and 5.2% respectively. For a blood loss greater than 1000 mL, they were 1.2% and 1.5% respectively.
In a study further analysing the data from their 2009 study, Dixon et al (2014) found women who had expectant management compared with active management received more treatment (use of an uterotonic drug) for excessive blood loss after birth. The relative risk of having treatment for excessive blood loss was 1.7 (95% confidence interval: 1.6–1.8) for women in the expectant management group compared to the active management group. However, once the women received a uterotonic drug to treat excessive blood loss, those in the expectant management group were less at risk of a postpartum haemorrhage compared with the active management group (relative risk: 0.54, 95% confidence interval: 0.5–0.6). Among women in the expectant management group, 3.7% had blood loss of more than 500mL, compared to 6.9% in the active management group.
Grigg et al (2017) compared clinical outcomes for women intending to give birth in a freestanding midwife-led unit (n=407) or a tertiary level unit (obstetric-led unit) (n=285) in New Zealand. All but 29 of the women intending to give birth in the midwife-led unit were identified as at low risk of obstetric complications and consequently, at low risk of postpartum haemorrhage; while 29 women were identified as at high risk of obstetric complications and consequently, at high risk of postpartum haemorrhage. The study found that despite higher proportions of women who intended to birth in the midwife-led unit choosing expectant management, compared with higher proportions of women who intended to birth in the tertiary level unit choosing active management, the overall rates of postpartum haemorrhage were similar (23.3% of women in the midwife-led unit, compared with 24.7% of women in the obstetric-led unit).
Fahy et al (2010) collected and analysed data on women classified as low risk of postpartum haemorrhage who gave birth at a freestanding midwife-led unit from July 2005 to June 2008 (n=361 after exclusions for postpartum haemorrhage risk factors) and at a tertiary level maternity unit (comprising an obstetric-led unit and an alongside midwife-led unit) from January 2006 to June 2008 (n=3436 after exclusions for postpartum haemorrhage risk factors). The study was conducted in New South Wales, Australia. At the tertiary maternity unit, active management of labour was the policy and almost universal practice. Expectant management was mainly practised at the freestanding midwife-led unit and midwives who worked there received extra training in this management approach. The study revealed that 11.2% (344 of 3075) of women who received active management (the intended management approach at the tertiary level unit) experienced a postpartum haemorrhage compared to 2.8% (10 of 361) of women who had expectant management (the intended management approach at the freestanding midwife-led unit). The difference was statistically significant (odds ratio: 4.4, 95% confidence interval: 2.3–8.4).
Laws et al (2014) conducted a matched pairs cohort study of women defined as at low risk of postpartum haemorrhage in New South Wales, Australia. Maternal outcomes for these women who intended to birth at midwife-led units were matched with women who intended to give birth at alongside hospital's obstetric-led units. Data were collected between 2001 and 2009 from the computerised maternity notes of 15 742 women, who intended to birth at the midwife-led units and met the study criteria, and from the computerised maternity notes of 66 190 women who intended to give birth in the alongside hospital's obstetric-led units during the same period. Postpartum haemorrhage incidence at the obstetric-led units was 10.6% compared with 8.6% at the midwife-led units. This difference was statistically significant (odds ratio: 0.79, 95% confidence interval: 0.74–0.85), despite a much higher rate in expectant management of the third stage at the midwife-led units (24.4 versus 2.0%).
Monk et al (2014) investigated specified maternal and neonatal outcomes in women at low risk of obstetric complications in New South Wales, Australia, comparing women giving birth in freestanding midwife-led units in regional and urban areas with women intending to give birth in tertiary level units. Data were collected from the computerised maternity notes of women who met the study criteria and booked to give birth at the freestanding midwife-led units (n=494) and the tertiary-level units (n=3 157), from 2010 over a 17-month period. Prevalence of postpartum haemorrhage on the freestanding midwife-led units was 9.7% compared to 15.4% on the tertiary level units, which was statistically significant (P=0.031) despite a higher incidence of expectant management for these women compared with women booked on the tertiary-level units (37.4% compared with 2.9%).
Begley et al (2011a) conducted a randomised controlled trial comparing midwife-led care (n=1101) versus consultant-led care (n=552) for women at low risk of childbirth complications in Ireland. The findings from the study were that despite an increase in expectant management at the midwife-led unit compared to the obstetric-led unit (12.4%, 137 of 1101 versus 0.2%, 1 of 552; relative risk: 68.69) there was no statistically significant difference in estimated mean blood loss during the third stage of labour or shortly after (323 mL (standard deviation 317 mL) vs 324 mL (standard deviation 401 mL), 95% confidence interval: 32.12–44.46) or the incidence of postpartum haemorrhage (13.1%, 144 of 1101 versus 13.6%, 75 of 552; relative risk 0.96, 95% confidence interval 0.74–1.25).
Kataoka et al (2018) conducted a study comparing numerous maternal and neonatal outcomes in midwife-led and hospital obstetric-led units in Japan, including postpartum haemorrhage (defined as blood loss of more than 1000 mL) during the third stage of labour or shortly after birth. The study consisted of 9588 women at low risk of obstetric complications who had a spontaneous vaginal birth in one of 19 birth centres (midwife-led units), or in one of two hospital obstetric-led units. Data for the study were collected from maternity computerised records for women who given birth in the midwife-led units from 2001 to 2006 (5379 women) and for women who birthed in the hospital's obstetric-led units from 2004 to 2006 and from 2008 to 2009 (4209 women).
The study found a higher incidence of postpartum haemorrhage (defined as blood loss of more than 1000 mL) in women who birthed on the birth centres (22.1%) where women received expectant management, compared to women who birthed on the hospital obstetric-led units (18.4%) where women received active management. This difference was statistically significant; (odds ratio 1.47, 95% confidence interval: 1.31–1.64, P<0.001). However, women with risk factors for postpartum haemorrhage identified by the National Institute for Health and Care Excellence (NICE, 2017), including maternal age of 35 or over, parity 4 or more, and baby's birth weight of 4 kg or more, received expectant management in the midwife-led units. Additionally, during the time the study was conducted, midwives working in the midwife-led units were not able to convert to active management if the woman experienced excessive blood loss. These factors may have led to an increase in blood loss during the third stage or shortly after for women who birthed on the midwife-led unit, where expectant third stage management approach was practised. Since this study was conducted, midwives practising at midwife-led units in Japan are now able to convert to active management, if women develop risk factors for postpartum haemorrhage or experience excessive blood loss during the third stage of labour or shortly thereafter.
Summary
This literature review identified nine studies that directly or indirectly compared blood loss in women receiving active or expectant management approaches during the third stage of labour and shortly after birth. Most women in these studies were identified as at low risk of postpartum haemorrhage and gave birth in a variety of birth settings, including midwife-led and obstetric-led units.
The studies by Davis et al (2012) and Fahy et al (2010) found higher incidences of postpartum haemorrhage with active management compared with expectant management in all birth settings. However, twice as many women receiving expectant management went on to have further (uterotonic drug) treatment for excessive blood loss compared with those receiving active management (Davis et al, 2012). Dixon et al (2014) found that women who received expectant management and had treatment for excessive blood loss (use of a uterotonic drug) after birth were then less at risk of having a postpartum haemorrhage than women who received active management.
The studies by Dixon et al (2009), Grigg et al (2017), Laws et al (2014) and Monk et al (2014) revealed a lower incidence of postpartum haemorrhage in midwife-led units, despite an increased rate of expectant management and a reduced rate of active management. This was in comparison to the obstetric-led units, where there was an increased rate of active management and a reduced rate of expectant management.
Begley et al (2011a) also found that despite an increase in expectant management in midwife-led units compared to obstetric units, there was no significant difference in estimated mean blood loss during the third stage of labour or shortly thereafter, or in the incidence of postpartum haemorrhage. Therefore, it can be inferred that expectant management did not lead to a higher rate of postpartum haemorrhage. However, Kataoka et al (2018) found a significantly higher incidence of postpartum haemorrhage (defined as blood loss of more than 1000 mL) in women, who birthed in midwife-led units, where women received expectant management, compared to the hospital obstetric-led units where women received active management. However, the generalisability of the findings of this study may be limited by the unknown effects of postpartum haemorrhage risk factors on postpartum haemorrhage incidence. Furthermore, the inability of midwives to convert to active management if excessive bleeding was observed during the third stage of labour reduces the generalisability of the findings of this study to the UK and other settings, where midwives convert to active management if blood loss during the third stage is perceived to be excessive.
Discussion
There is a lack of studies that directly compare the incidence of postpartum haemorrhage in women at low risk of postpartum haemorrhage receiving active or expectant management while giving birth in midwife-led units, with no identified studies having been conducted in the UK. Only two studies were identified that directly examined the incidence of postpartum haemorrhage and active verse expectant management in women at low risk of postpartum haemorrhage giving birth in midwife-led units (Fahy et al, 2010; Davis et al, 2012). One of these studies, a large national study, only examined the incidence of severe postpartum haemorrhage (defined as blood loss of more than 1000 mL) (Davis et al, 2012). The other study (Fahy et al, 2010) was a small-scale study in which the low numbers of women may mean this study has limited reliability, validity and generalisability of the study's findings.
The studies identified in this review were also of varying quality and their generalisability to women at low risk of postpartum haemorrhage who have a physiological birth in midwife-led units in the UK is limited. The studies identified in this literature review were not stated as evidence by international (WHO, 2012; 2018) or national third stage of labour practice guidelines (RCOG, 2016; NICE, 2017; Royal College of Midwives, 2018); and were not included in Cochrane Reviews (Prendiville et al, 2000; Begley et al, 2010; 2011b; 2015; 2019) comparing active and expectant management. One reason for not being included as evidence or included in these Cochrane Reviews may have been that eight of the studies identified in this literature review were cohort studies. The evidence informing international and national third stage of labour practice guidelines and the Cochrane reviews comparing active and expectant management only include randomised controlled trials. This is because these trials are held as the gold standard for evaluating the effectiveness of interventions (Torgerson and Torgerson, 2008; Schulza et al, 2010).
It has been questioned whether a randomised controlled trial is appropriate to investigate an expectant third stage of labour management approach and any associated blood loss (Fahy, 2009). This is because for a woman to participate in a randomised controlled trial investigating an expectant third stage of labour management approach and associated blood loss, she should be randomised after the birth of the baby. At this point it will be known if she has had a spontaneous vaginal birth and is at low risk of postpartum haemorrhage. This is essential, as expectant management is only appropriate for women who have had a normal physiological birth and are at low risk of postpartum haemorrhage. However, Fahy et al (2010) also comment that to randomise women after the birth of their baby would be unethical because of difficulties regarding obtaining informed consent. It has also been commented that asking women to think about taking part in a study and give their informed consent during this stage of labour, might be an intervention that disturbs their hormones and impacts on the birthing process, including the birth of the placenta and membranes (Edwards and Wickham, 2018). Consequently, to conduct a randomised controlled trial to investigate an expectant third stage of labour management approach and any associated blood loss during the third stage or shortly after might not be appropriate.
Cohort studies reflect more accurately what is happening in practice, as the researcher does not intervene in practice but observes it (Hackshaw, 2015). Although cohort studies can also be more susceptible to confounding bias, as participants are not assigned randomly to intervention groups and, as a result, their outcomes may differ. These differences may not be entirely because of the intervention, but because the participants or their circumstances may be inherently different from the start (Greenhalgh, 2019). Additionally, researchers in retrospective cohort studies can only use data that has already been collected, so there may be a greater potential for missing data (Greenhalgh, 2019). These issues may reduce validity and reliability and increase bias in these types of studies (Greenhalgh, 2019).
Conclusions
This review suggests that for women at low risk of postpartum haemorrhage who choose to birth in a midwife-led unit and want to experience a birth with minimal interventions, an expectant third stage of labour approach is a reasonable option. When healthcare professionals are discussing third stage of labour care with women, they need to review the evidence practice that guidelines are based on and evaluate whether they are generalisable to each woman under their care. Healthcare professionals should not be intervening in pregnancy and childbirth without high-quality evidence to support that intervention and without the woman making an informed choice.
There is a need for further research studies investigating third stage of labour management approaches and any related blood loss during this period or shortly after in women who had a normal physiological birth and give birth in a midwife-led unit. This is because research studies have reported many beneficial outcomes for healthy women at low risk of obstetric complications, who plan to birth in midwife-led units.
Key points
- Research studies informing third stage of labour practice guidelines and recommendations are questionable, particularly for women at low risk of postpartum haemorrhage who choose to give birth in midwife-led units.
- This literature review found limited studies of varying quality that investigated active versus expectant management and any related blood loss in women at low risk of postpartum haemorrhage who had a normal physiological in a midwife-led unit.
- The generalisability of the studies identified in this literature review to women at low risk of postpartum haemorrhage who have a physiological normal birth and give birth in midwife-led units in the UK is limited.
- More studies are needed as research studies have reported many beneficial outcomes for women at low risk of obstetric complications, who choose to birth in midwife-led units.
CPD reflective questions
- Do you think your third stage of labour practice guideline is generalisable to women at low risk of obstetric complications who choose to birth away from a hospital obstetric-led unit?
- How have you come to this conclusion?
- When was the last time you questioned the evidence practice guidelines are based on?
- When was the last time you reviewed the evidence practice guidelines are based on and assessed if they are generalisable to the woman you are providing care for?


